Whole person care is gradually becoming more prevalent in the realm of health and human service organizations. But what exactly does it mean? Check out the definition and importance of whole person care, as well as how your organization can begin implementing it today.
What is Whole Person Care?
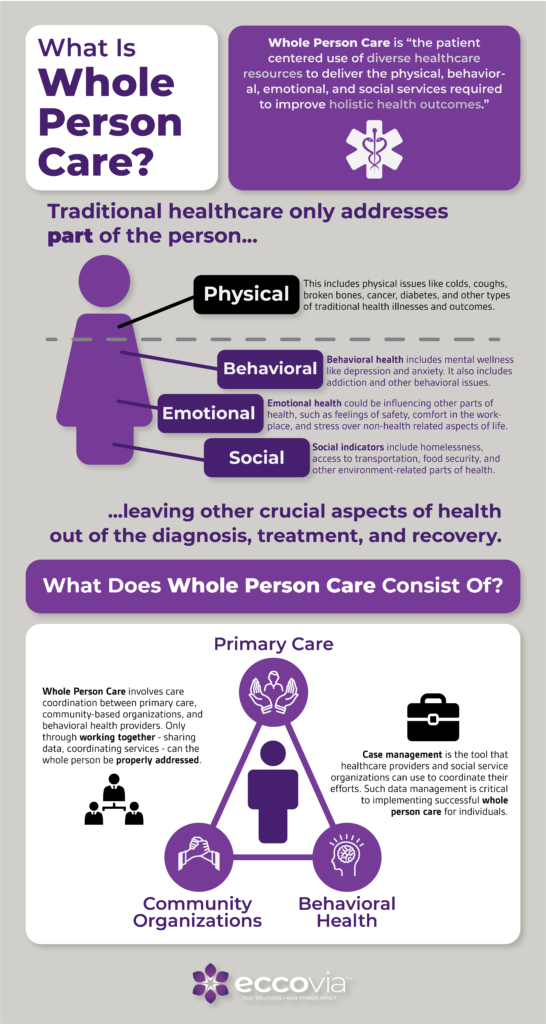
When someone arrives at a doctor’s office or service center, they are bringing along more than just their physical body. This person’s emotional, social, mental, spiritual, and behavioral needs have just as much of an impact on their overall physical health. Addressing all parts of their situation—not just the traditional, physical ones—is known as whole person care.
Oftentimes, individuals in lower socio-economic brackets—and therefore those who rely most on social services—experience more adverse social determinants of health. These determinants (like access to healthy foods, literacy level, and community environment) often impact the non-physical side of health. By incorporating whole person care into social services, providers can better address needs and improve overall outcomes.
Check out the infographic below for a breakdown of what whole person care consists of.
Why is Whole Person Care Important?
The better we understand what whole person care is, the better we can see why it is important.
Essentially, whole person care is critical because research shows that addressing only one part of the person only solves part of the issue. Conversely, complete human wellness relies on a multi-dimensional approach to make lasting changes.
Researchers at the Weill Cornell Medicine found that whole person care can help doctors more accurately predict fatal coronary heart disease in their patients. By looking at the social, behavioral, and emotional factors facing these individuals, such as access to transportation and civic participation, medical experts could better assess the whole person.
Some experts argue that lower health outcomes in the US may be due to our “medicalized” approach. While we focus on medical interventions, our systems traditionally ignore other factors that can have a much larger impact on health outcomes.
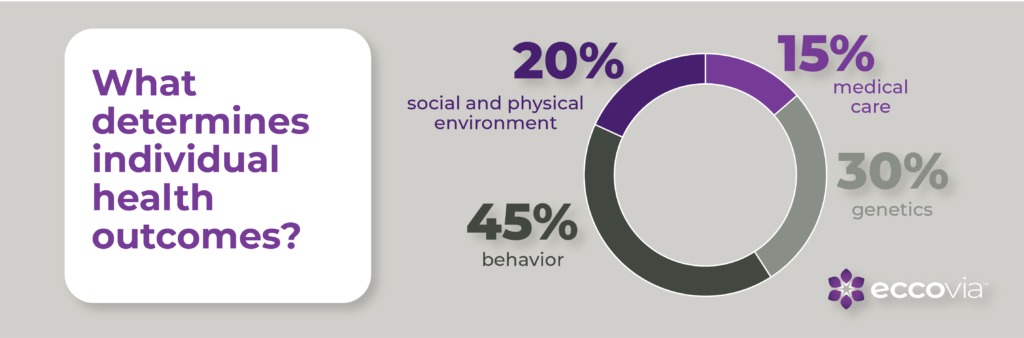
The American Action Forum reports that, although 95% of health spending goes toward medical care, it only accounts for about 15% of an individual’s health. Social and physical environment, key pieces of whole person care, make up 5 percent more of our health than traditional care, and behavior is more than both of those combined.
Understanding exactly what accounts for an individual’s health outcomes helps us see why traditional care is simply not enough. For those who are more reliant on social services for their health, whole person care is even more critical for successful wellness.
How to Implement Whole Person Care
The best news about whole person care? You and your organization can begin implementing it today. The more we can broaden our perspective to include other aspects of health and human services, the better we can treat the whole person. Consider the “Three C’s” of implementing whole person care below.

Additionally, you may want to consider 7 Ways Your Program Can Start Implementing Whole Person Care. In this blog post, we go in depth about how your organization an incorporate coordinated care.
Eccovia is committed to using whole person care to better health and human services, which is why our case management platform ClientTrack™ is an industry leader for whole person care. We help programs record data, analyze it in meaningful ways, and coordinate with other community services to maximize impact.
The more we understand about whole person care, the more effective our programs can become. Treating the whole person—all aspects of them—helps create a more substantial whole person care approach, which in turn better serves each individual.
Reach out today to learn more about whole person care and how you can include it today.
Enjoy This Article? Then You’ll Like:
Caring for the Whole Person: How Do We Address Stress?



