ClientConnect 2023, our inaugural peer-to-peer conference for human services organizations, was a resounding success! But if you missed out, don’t let that stop you from catching the next one. In the follow-up to this article, we’ll explore the ClientConnect presentations from ICF and Health Roads, so you know what to expect next time for ClientConnect 2024.
It really “takes a village” when it comes to helping social services succeed in their mission to mitigate suffering and end homelessness. Another apt saying that illustrates this principle: “If you want to go fast, go alone. If you want to go far, go together.” Eccovia is interested in advancing community outcomes through collaboration. However, social service organizations often need additional capabilities when it comes to improving processes, putting together the perfect request for proposal (RFP), deciding what technology they need, and organizational strategy.
That’s where ICF and Health Roads, partners of Eccovia, come in. These organizations not only consult and help communities manage their projects—they also help them understand the social service landscape. Health Roads provides:
- Expertise and capacity building
- Customized support and software
- Promotion of best practices
- Resource allocation and management
So how does Eccovia partner with ICF and Health Roads? Together, we identify strategies and capabilities that enable communities’ data infrastructures to support better outcomes. For example, ICF’s expertise in navigating governance and related policy challenges complements Eccovia’s expertise in the technology infrastructure that makes community care coordination possible, while our partnership with Health Roads is focused on the collective community impact that comes from bridging social and health services data.
Health Roads: Medicaid Billing for Non-Medical Service Organizations
“We make sure your services and your organizations continue to receive money from a stable revenue stream,” said Rajib Ghosh, CEO of Health Roads. Health Roads is a nationally growing business that works with social care, community-based organizations (CBOs), addressing needs in various segments, including but not limited to:
- Refugee resettlement
- Immigration
- Youth development
- LGBTQ+ services
- Cancer networks
- Substance abuse
- Inmate re-entry
Current State of Medicaid Expansion and Section 1115 Waivers
Social services and health services are becoming more interdependent, with the realization that the social determinants of health (SDoH) outcomes of vulnerable populations can improve more often when these services work together via community care coordination. That’s where the Medicaid 1115 Waiver Program comes in.
Put simply, the Medicaid 1115 Waiver Program unlocks additional funding not possible through other means. It also represents the evolution of care taking place in communities, which will increasingly involve social and health services providers working together. This coordination is the basis for whole-person care, social determinants of health (SDoH)–focused care, and holistic care.
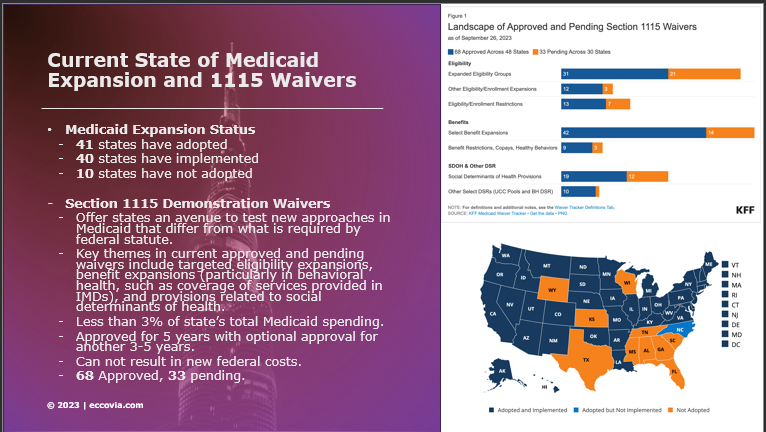
Source: Health Roads, Eccovia.
Health Roads’ software and consulting services allow communities to unlock the funding that is available from the 1115 program, to help states and communities innovate the interaction and coordination between healthcare and human services. Under the 1115 waivers, states can implement changes in Medicaid for a limited period (usually 5–10 years), subject to federal approval. These changes can include adjustments to their social programs’ design, beneficiary eligibility, service delivery, and payment methods. The primary objective is to improve care, increase efficiency, and reduce costs.
Substance use disorder, homelessness, and mental/behavioral health are the primary three needs the 1115 waiver program addresses, but it could also address youth services, to aging and long-term care-based programs, plus more.
Behavioral health, physical health, housing, and other social benefits are intersecting now at the policy level, but the technology solutions that enable this coordination of services aren’t catching up. It’s one of those rare instances where policy is outpacing technology, while it’s usually the other way around, Ghosh explained.
It’s also true that more Medicaid services will be administered via managed care, and non-medical organizations are being asked to participate in managed care networks.
Examples of 1115 Waiver Programs
So how are states taking advantage of this funding opportunity? One prime example is Washington, which received a large waiver from CMS to assist in care coordination for inmate re-entry. California is using the waiver program to redesign their entire Medicaid program (Medi-Cal) to include many social services, with housing as a large part. Minnesota’s program is targeting primarily substance abuse, among other factors.
When community-based organizations (CBOs) take advantage of this decade-long funding stream, you’re less reliant on philanthropic fundraising, which often occurs every two years and takes up lots of effort with grant writing and so forth.
There’s one big caveat to this program, however: You have to work within the framework that CMS provides. “That is not trivial,” Ghosh pointed out. “Either you have to work with a managed care organization [MCO], like Kansas is going toward,” or you have to work with managed care health plans (MCPs).
Billing Solution for Non-Medical Businesses
Most housing providers aren’t familiar with how to bill, while medical clinics are. What do you do when a claim is rejected by an insurance company? How do you deal with the appeal process? How do you get prior authorization?
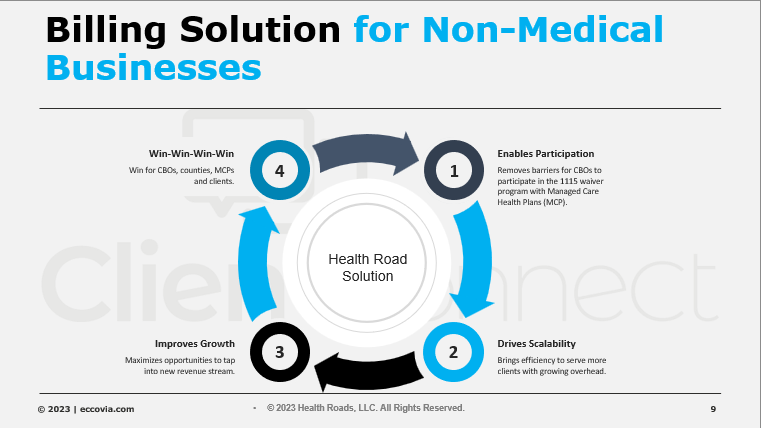
Source: Health Roads, Eccovia.
Health Roads wants to enable CBOs to participate in the healthcare billing model so nonprofits can drive scalability and serve more people, without having to worry about their costs outpacing their revenue.
For example, a state government is not going to accept a bill from anyone, so the MCP needs to operate within the framework used for patients visiting health providers. Ghosh explained further: “A clinic knows how to send a claim to insurance, but a housing provider doesn’t know how to do that. A housing provider doesn’t know what to do when a claim is rejected by an insurance company or how to deal with that. . . . By the way, you need prior authorization to provide a service if you are participating in managed care.”
California County Case Study
One county in California acts as a community hub to enable housing service providers and medically-tailored meal CBOs to participate in the 1115 waiver program, called CalAIM. To that end, Health Roads concepted and built a solution for translating HMIS services into claims and encounters for the managed care plans of the county.
“Our goal is to minimize the time from first service to cash payment,” Ghosh clarified, “to minimize the amount of denials.” After Health Roads’ involvement with this county, CBOs benefitted with capped and fee-for-service revenue contracts with MCPs. Depending on the size of those CBOs, 100,250 clients could be served per month with the waiver-funded reimbursable services, like tenancy sustaining, housing navigation, and housing deposits.
As another result of this effort, $12 million in additional revenue was distributed to those CBO organizations who enrolled.
Functional Capabilities of Health Roads
If you are working through a managed-care organization (MCO), you have to take authorizations before you can render services, so you need to connect authorization with service claims.
This requirement might be burdensome and impede service delivery without a smooth billing process, but that’s where Health Roads comes in. In the HMIS system, there’s already capability to do many layers of reporting, but there’s no functionality for healthcare billing or Medicaid billing, but Health Roads has developed functional capabilities that make this functionality possible.
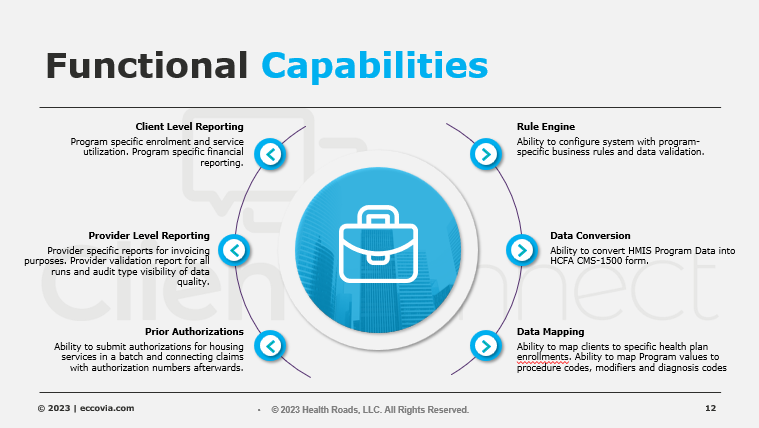
Health Roads’ technology has developed to include these features. Source: Health Roads, Eccovia.
Billing Workflow for 1115 Waivers and Social Services
This billing workflow for the California county (mentioned above) includes Health Roads’ “secret sauce,” which works for many social services, including medically-tailored meals and more.
This workflow receives information through various means, sometimes through databases or flat file exports, and Health Roads combines those ingestions into its solution. This solution also accommodates “retroactively entered services,” for example, a client who’s been retroactively enrolled in a health plan, in a 90-day evaluation cycle. They also identify clients whose services have not been rendered for one reason or another.
HMIS program data are then converted into procedure codes, diagnoses codes, modifiers, and even billing rules.
For example, if you have multiple service programs, you need to be able to flag potential duplicate services so you’re not reporting bad data, and the same thing goes for timely filing: these services need to be eligible for submission if they’ve not been lingering around for longer than 180 days.
From there, multiple scenarios ensued in this California example:
- One organization had populations in multiple health plans, and while one plan wanted information to be submitted in electronic data interchange (EDI-837) format, which is standard for healthcare, while the other plan wanted an Excel spreadsheet with the information laid out in an invoice style. Health Roads generated those outputs and submitted them along with each health plan, as well as the corresponding reporting (i.e., number of clients submitted, missed services, utilization rate). Then those reports/claims were sent to the health plans in their requested formats.
- Health Roads also helped the organization identify clients for whom there were no matching enrollments with health plans. Either the record was stored for use in the next run of the billing workflow, or a “no health plan” invoice was sent to the county agency.
This workflow runs at a monthly basis usually, because it’s more comprehensive than a weekly basis, but CBOs can customize that.
The Current State of Affairs with Health and Social Care Integration
Most social care platforms are not set up for integrating with healthcare; “ClientTrack, however, is set up for that,” Ghosh reminds us. He also reminded us that electronic health record (EHR) systems are not fully set up for SDoH factors, which means social care CBOs are not usually working within the managed care framework, because working within the managed care framework is administration heavy, cost intensive, and therefore difficult for non-medical CBOs.
Concluding Thoughts
Because the 1115 Waiver Program allows for integration between social and healthcare, MCOs and CBOs find themselves in a unique situation, as stated above: policy and funding opportunities are getting ahead of the technology solutions currently available.
That’s why Eccovia and Health Roads have partnered together—to help communities increase their cross-sector collaboration.
If your community would like to take advantage of the Medicare and Medicaid 1115 Waiver Program but need technical assistance in doing so, Health Roads is available to schedule a conversation.
If your community would like to see how ClientTrack facilitates better community care coordination, in addition to facilitating the capabilities Health Roads provides, schedule a demo with Eccovia’s experts.
After all, SDoH outcomes are no longer just in the domain of social services. Now is the time for all human services to work together to provide the critical needs of vulnerable populations.



