Despite being high-risk for COVID-19 complication, HIV/AIDS patients still experience challenges in obtaining the care they need. As organizations better understand the relationship between HIV and the coronavirus, it emphasizes the need for community care coordination.
COVID-19 Is Not the Only Pandemic
As the US hits its one-year mark dealing with COVID-19, many Americans are still struggling. Food insecurity, homelessness, and unemployment are all on the rise, with no end in sight. For those experiencing additional health disparities—such as HIV or AIDS—the difficulties are even greater.
The first cases of AIDS in the US were reported in 1981. Since then, over 700,000 Americans have died from the disease—and thousands continue to die each year.
In a similar fashion to the coronavirus, HIV/AIDS impacts each community differently. In fact, there is a strong correlation in diagnoses among minorities and those with lower socio-economic statuses. Many experts point to social determinants of health as crucial to understanding and helping those living with HIV/AIDS.
“We have incredible tools to prevent and treat HIV, but people may not fully utilize them if they are facing personal or structural issues that pose more immediate hardship like substance use and mental health disorders,” states Chris Beyrer, MD, in a recent press release. “You may struggle to take a daily medication if you are facing food insecurity or cannot find affordable treatment for your substance use disorder.”
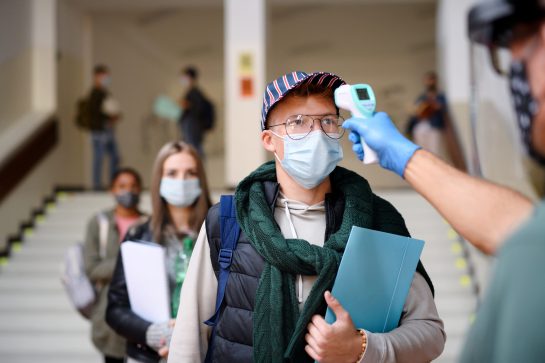
Being HIV-Positive in the Era of Coronavirus
While barriers for those with HIV have always existed, the coronavirus epidemic has only magnified these issues. When quarantine was first instituted back in March 2020, many clinics were unprepared to go virtual. HIV/AIDS patients require daily medications to stay alive, and many feared being unable to access such vital treatments.
Again, social and health disparities were at work against HIV patients. As many still face discrimination in the workplace and are unemployed, some patients are unable to afford the technology needed for telehealth visits.
Other HIV-positive individuals have reported feeling neglected during the pandemic. Despite the critical, life-saving nature of HIV/AIDS treatment, some worry the stigma surrounding this disease continues to divert medical attention away from HIV patients, even when they need it most.
“The pandemic may have exacerbated gaps already present in the HIV space,” notes Maggie Shaw of AJMC.

Approximately 1.2 million people in the U.S. are living with HIV today.
Is There a Cause for Concern?
Not only are HIV patients concerned about receiving their traditional treatment—they may also be more at risk for COVID-19.
While data on the coronavirus is still proving difficult to effectively analyze, many experts note the unequal burden on HIV patients. A recent US study found that those with HIV/AIDS who contract COVID-19 are 40% more likely to be hospitalized. In the UK, those with both HIV and coronavirus were 3x more likely to die, and HIV-positive COVID-19 patients were significantly younger than HIV-negative COVID-19 patients.
For those who have progressed from HIV to AIDS, the risks are even greater. With lower immunity, a positive COVID-19 result could prove deadly for such patients.
A Gap in Care Coordination
Although there is evidence suggesting HIV patients need additional care for COVID-19, many still struggle to obtain it.
Just last month, a 59-year-old man with AIDS was denied the vaccine in Philadelphia. Despite his diagnosis meeting Pennsylvania’s criteria for high-risk vaccine eligibility, the man was still turned away from his local Walgreens.
“I’ve survived AIDS for 30 years, and I definitely don’t want to die now from COVID,” the man (whose identity is withheld to protect his privacy) told the Philadelphia Gay News. “I don’t understand why the city appears to be so resistant to doing the right thing.”
This Pennsylvanian man’s experience highlights just one of the many difficulties HIV/AIDS patients face in the current health system. Despite being told they qualify for the vaccine, many still experience barriers due to stigma and misinformation. It highlights that now, more than ever, HIV-positive individuals need effective community care coordination.
“Scientific advances have transformed the course of HIV in individuals. To transform the course of the epidemic, we need to expand care and prevention strategically to those who need it most,” said National Institute on Drug Abuse Director Dr. Nora D. Volkow.
Community care coordination can effectively bridge these gaps that historically HIV/AIDS patients have had to navigate by themselves. Through effective communication between non-profits and other service providers, coordinators can ensure that patients (like the man from Pennsylvania) receive the care they need. Even if programs do not offer special care for HIV-positive individuals, care coordination can make sure that clients are referred to organizations that do offer specialized treatment.
Effective community care coordination is best achieved through case management systems like ClientTrack™. ClientTrack can seamlessly integrate data between organizations, making coordination quick and easy. For HIV/AIDS patients, effective case management is critical to their survival.
ENJOY THIS ARTICLE? YOU MAY ALSO LIKE:
What Can Your Program Do To Help Eradicate HIV/AIDS?
How to Stop STDs? The Answer Lie in SDoH
Sources Used:
- https://www.news18.com/news/buzz/ask-the-doctor-does-covid-19-pose-a-greater-risk-to-those-living-with-hiv-aids-3483494.html
- https://www.ajmc.com/view/hiv-care-continuum-strained-under-covid-19-pandemic
- https://www.poz.com/article/concerns-covid19-hiv
- https://www.poz.com/article/man-aids-denied-covid19-vaccine-philadelphia
- https://www.thehansindia.com/telangana/hiv-cases-dropped-during-lockdown-in-telangana-674628
- https://link.springer.com/article/10.1007/s11904-021-00543-4